Media
HKUMed unveils the novel function of extracellular vesicle in driving liver cancer metastasis, providing new targets for early diagnosis and treatment
31 Aug 2020
Dr Judy Yam Wai-ping, Associate Professor of the Department of Pathology, HKUMed (left), with her research team members, Dr Tey Sze-keong, Post-doctoral Fellow (right) and Ms Cherlie Yeung Lot-sum, Research Assistant (middle).
A research team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that the liver cancer cell-derived extracellular vesicles (EVs) promote tumour growth and metastasis to lungs. The novel findings of the tumour-derived extracellular vesicles provide insights into promising biomarker and new therapeutic approach for liver cancer.
A research team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that the liver cancer cell-derived extracellular vesicles (EVs) promote tumour growth and metastasis to lungs. The novel findings of the tumour-derived extracellular vesicles provide insights into promising biomarker and new therapeutic approach for liver cancer.
A research team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that tumour-derived extracellular vesicles promote liver cancer metastasis. The novel findings of the tumour-derived extracellular vesicles provide insights into promising biomarker and new therapeutic approach for liver cancer. The ground-breaking findings have been published in the leading multidisciplinary science journal, Advanced Science. [link to the publication]
Background
Liver cancer is one of the most prevalent cancers worldwide with an incidence of over 840,000 new cases. It is highly prevalent in Hong Kong and Mainland China. In Hong Kong, the newly diagnosed cases are approximately 1,800 per year and liver cancer accounts for over 1,500 cancer deaths per year. About 8% of Hong Kong population are hepatitis B virus (HBV) carriers while 80% of liver cancer patients are related to HBV infection. The high mortality rate of liver cancer is primarily attributed to late presentation, frequent recurrence and metastasis. Most late stage patients are inoperable and have very limited therapeutic options, laying emphasis on the need to identify promising biomarkers for early diagnosis and to develop new treatments for cancer patients.
Research findings
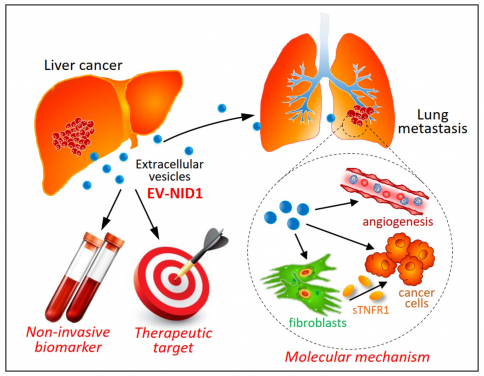
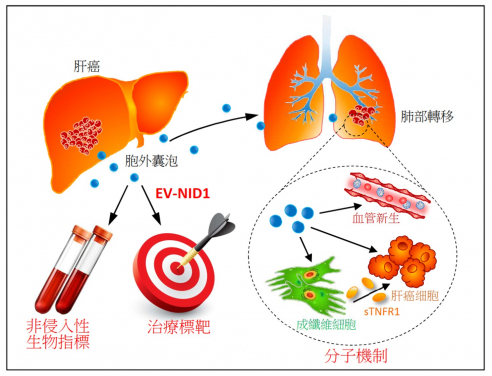
Using the mouse model of liver cancer, the research team found that the liver cancer cell-derived extracellular vesicles (EVs) promote tumour growth and metastasis to lungs. The team further discovered that the nidogen 1 (NID1) present in EVs is crucial for the promoting effect of EVs. Functionally, EV-NID1 enhances angiogenesis and activates fibroblasts to secrete tumour necrosis factor receptor 1 (TNFR1), facilitating lung colonisation of tumour cells. EV-NID1 also augments tumour cells to proliferate, migrate and invade. Knockdown of NID1 expression in EVs drastically reduces the promoting effect of EVs. The application of anti-TNFR1 antibody effectively diminishes lung metastasis induced by liver cancer cell-derived EVs in mice. In the clinical perspective, serum EV-NID1 and TNFR1 levels are higher in liver cancer patients than control individuals.
“Our study provides the first evidence about the presence of NID1 in extracellular vesicles of liver cancer patients and demonstrates its previously unknown functions in driving liver cancer development and metastasis. We envisage the blockage of the functions and signalling pathways of tumour-derived extracellular vesicles can be applied as a therapeutic approach for cancer patients in the future,” said Dr Judy Yam Wai-ping, Associate Professor of the Department of Pathology, HKUMed, who led the research.
Significance of the study
The findings of the study have significant implications in clinical applications. Firstly, the identification of the molecular driver of liver cancer is fundamental to the design of novel therapeutic interventions to eradicate this deadly disease. Secondly, the levels of serum EV-NID1 and TNFR1 are positively associated with the tumour stages of liver cancer patients, suggesting the potential application of these molecules as non-invasive biomarkers for the early detection of liver cancer. Thirdly, the study offers promises for the new direction of liver cancer treatment by targeting oncogenic EV components and their mediated pathways to benefit liver cancer patients in the long term.
About the research team
The research was led by Dr Judy Yam Wai-ping, Associate Professor of the Department of Pathology, HKUMed. Dr Mao Xiaowen and Dr Tey Sze-keong, Post-doctoral Fellows, Department of Pathology, HKUMed are co-first authors, assisted by Ms Cherlie Yeung Lot-sum and Mr Ernest Kwong Man-lok, Research Assistants of Dr Yam’s team. Collaborators include Dr Eva Fung Yi-man, Mass Spectrometry Facilities Manager, Department of Chemistry, HKU; Dr Clive Chung Yik-sham, Assistant Professor of the Department of Pathology and School of Biomedical Sciences, HKUMed; and from the Department of Medicine, HKUMed: Dr Danny Wong Ka-ho, Assistant Professor, Dr Loey Mak Lung-yi, Clinical Assistant Professor, Dr James Ho Chung-man, Clinical Associate Professor and Professor Yuen Man-fung, Deputy Head of Department, Li Shu Fan Medical Foundation Professor in Medicine, Chair of Gastroenterology and Hepatology; Dr Herbert Pang Hei-man, former Associate Professor of the School of Public Health, HKUMed; Dr Maria Wong Pik, Principal Clinical Practitioner of the Department of Pathology, HKUMed. Collaborating institutions contributing to the research include The Hong Kong Polytechnic University, Queen Elizabeth Hospital and Southern Medical University, Guangzhou.
The work was supported by Hong Kong Research Grants Council (#17117519).
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email
(medmedia@hku.hk).
