Media
HKU dietetics research identifies low GI diet
a potential Type 2 diabetes prevention strategy
07 Dec 2020
Type 2 diabetes is a lifelong condition that causes blood sugar level to become too high and the complications could be life-threatening. Great fluctuations in post-meal blood glucose levels is suggested to be a contributing factor of type 2 diabetes development. Therefore, reducing post-meal blood glucose fluctuation is believed to be beneficial for type 2 diabetes prevention.
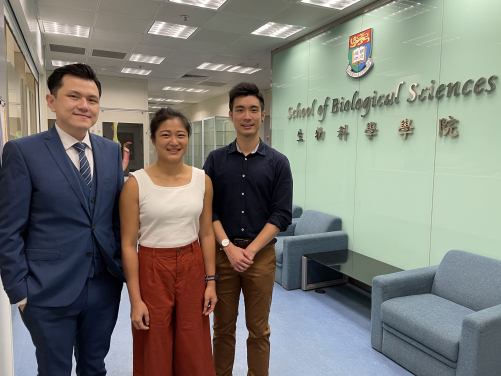
In a recent study of the research team from the Research Division for Molecular & Cell Biology of the University of Hong Kong (HKU), led by Assistant Professor Dr Jimmy Chun Yu LOUIE and consisted of graduate researcher Dr Tommy Hon Ting WONG and student researcher Hannah Wing Han HON, performed a research comparing the overall fluctuations in blood glucose levels of a high GI diet and a low GI diet for a 10-day trial period, which is the longest ever among research of the same type.
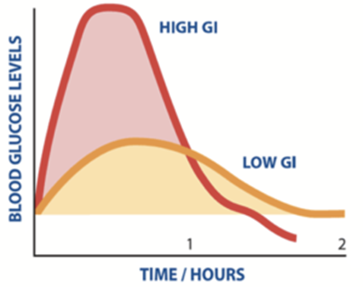
The study team recruited 14 healthy adults aged from 19 to 25 years' old and had them follow either a low or high GI diet for 5 days. Then they reverted to their normal diet for at least 2 days, followed by the opposite diet plan for another 5 days. All diets contained 5 meals (3 main meals and 2 light snacks). The high GI diet mostly contained simple and refined carbohydrates including muffins, white rice and potato, which will be digested and absorbed quickly, resulting in a rapid rise in post meal blood glucose levels. On the other hand, the low GI diet mostly contained complex carbohydrates and unprocessed foods, such as wheat bran, buckwheat noodles, oat, and brown rice. These foods are digested and absorbed more slowly, thus having a lower impact on post meal blood glucose levels (See note 1).
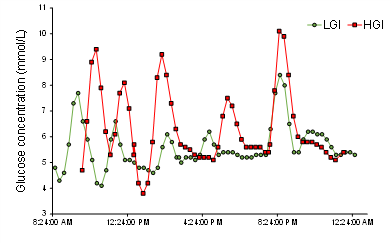
The team found that following the low GI diet, the overall fluctuations in blood glucose levels during the day was 15 % lower than that of following the high GI diet. This study also monitored the blood glucose levels of the participants on a daily basis, and the results of the study provide direct evidence to support the use of a low GI diet to reduce the risks of developing glucose intolerance.
15% lower in blood glucose levels
The Glycemic Index (GI) is a ranking of the overall impact of different foods (in portions with the same amount of carbohydrates) on blood glucose levels after their consumption, where foods with lower GI would have a lower impact as they are digested and absorbed more slowly than higher GI counterparts. A recent meta-analysis of randomised controlled trials by Ojo et al.(See note 2) concluded that following a low GI diet to avoid glucose fluctuation can improve blood glucose control in patients of type 2 diabetes better than a higher GI diet. However, the effect of following a low GI on the daylong variation of glucose levels in healthy adults, and hence its potential as a type 2 diabetes prevention strategy, has not been assessed before.
The research team found that, compared with a high GI diet, when following the low GI diet, the overall fluctuations in blood glucose levels during the day was 15 % lower than that of following the high GI diet. The peak blood glucose levels after having breakfast and afternoon snack were also lower when following the low GI diet, while no statistically significant differences between the two diets were observed for lunch and dinner. The more pronounced differences in breakfast could be due to the higher sensitivity of blood glucose level to carbohydrate intake in the morning; while for snacks it could be due to difference in food choices and handling. (A sample 1-day menu for each diet is provided here)
Research methodology: Standardised diets to improve accuracy
The study aimed at comparing the variation in glucose levels between consuming diets low and high in GI. To control for the potential effects of other macronutrients on day-long glycaemia, the LGI and HGI meals in our study were designed to be matched for macronutrient and fibre content: around half of the energy intake was contributed by carbohydrates, while fat and protein each contributed a quarter. The only difference between the two diets was the GI: the HGI diet had a 20-unit difference in GI compared with the LGI diet.
The low GI and high GI diets were designed by registered dietitians and all foods were cooked and delivered by a commercial meal delivery service. One of the strengths of this study is that all of the foods consumed by the subjects were provided, and all subjects had standardised diets, ensuring good compliance with the assigned dietary GI, thereby ensuring the nutritional qualities of the diets.
The blood glucose levels of the participants when they were on the diets were monitored using a flash glucose monitor system. It worked by having a sensor inserted at the back of the upper arm of each participant. The sensor automatically records the glucose level in the interstitial fluid every 15 minutes during the day. Hence it was able to generate records of glucose levels for each participant every day during the experiment period.
When compared with previous studies of low GI diets, the study by Dr Louie is the first to provide participants with all the foods in the experiment for a 10-day trial period, which is the longest period over which a low GI diet has been studied meal-to-meal in comparison with a matched high GI diet. This study also monitored the blood glucose levels of the participants through each day of the experiment period, thus the analysis of the glucose fluctuation during the day was possible. Results of this study provide direct evidence to support the use of a low GI diet to reduce the risks of developing glucose intolerance.
Link to the Journal paper: https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/dom.14167
Note 1: Search engine for the Glycemic Index by The University of Sydney: https://www.glycemicindex.com/index.php
Note 2: The Effect of Dietary Glycaemic Index on Glycaemia in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials: https://pubmed.ncbi.nlm.nih.gov/29562676/
For media enquiries, please contact Ms Casey To, External Relations Officer of HKU Faculty of Science (tel: 3917 4948; email: caseyto@hku.hk) /Ms Cindy Chan, Assistant Director of Communications of HKU Faculty of Science (tel: 3917 5286; email: cindycst@hku.hk) or Dr Jimmy Louie, Assistant Professor of Research Division for Molecular & Cell Biology (tel: 2299 0677; email: jimmyl@hku.hk).
Image download: https://www.scifac.hku.hk/press